Title Page
-
Conducted on
-
Prepared by
-
Location
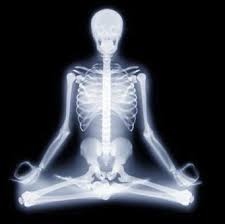
§482.26(a) Standard: Radiologic Services
-
The hospital must maintain, or have available, radiologic services according to the needs of the patients.
-
A hospital’s diagnostic radiologic services must be maintained or available at all times.
-
Multi-campus hospitals must have diagnostic radiologic services that can be furnished when needed in a clinically appropriate timeframe for each location providing inpatient, same-day surgery, and emergency services.
-
The scope and complexity of diagnostic radiological services maintained or available must be specified in writing, in order to demonstrate how the hospital meets the needs of its patients.
-
Radiological services may be provided by the hospital directly utilizing its own staff, or through a contractual arrangement. The hospital is responsible for ensuring that the services meet all the requirements of this regulation, regardless of whether they are provided directly or under arrangement.
-
Teleradiology is acceptable, so long as the teleradiology practitioner is privileged in accordance with the requirements of the Governing Body (§482.12) and Medical Staff (§482.22) CoPs.
-
The patient is properly identified to ensure that the ordered radiology test is performed on the correct patient.
-
Patients are educated regarding x-rays and other radiological procedures.
§482.26(b) Standard: Safety for Patients and Personnel
-
There are written hospital policies and procedures and protocols for specific radiologic services modalities that are based on identified professionally approved standards, and which address the ALARA principle as well as the other safety and risk-reduction measures.
-
The safety protocols are reviewed periodically and, if applicable, updated.
-
The radiologic services staff are familiar with the policies and procedures related to safety in general and specific clinical protocols.
-
The policies and procedures are followed when radiologic services are delivered to patients.
-
The radiologic services staff are trained at appropriate intervals to ensure that they are operating the equipment according to manufacturer’s instructions and hospital policy
-
The radiologic services staff know how to respond to adverse events.
-
The areas where radiologic services are provided are equipped with the equipment or materials to immediately respond to an adverse event.
-
The hospital monitors the quality and safety of radiologic services.
-
Adverse events are analyzed for their causes and preventive actions are taken.
§482.26(b)(1) - Proper safety precautions must be maintained against radiation hazards. This includes adequate shielding for patients, personnel, and facilities, as well as appropriate storage, use and disposal of radioactive materials.
-
The hospital must adopt and implement written policies and procedures to ensure safety from radiation hazards. The policies and procedures must include, but are not limited to, consideration of the following:<br>• Clear and easily recognizable signage identifying hazardous radiation areas;
-
The hospital must adopt and implement written policies and procedures to ensure safety from radiation hazards. The policies and procedures must include, but are not limited to, consideration of the following:<br>• Limitations on access to areas containing radiologic services equipment.
-
The hospital must adopt and implement written policies and procedures to ensure safety from radiation hazards. The policies and procedures must include, but are not limited to, consideration of the following:<br>• Appropriate use of shielding, including:<br>• Types of personal protective shielding (e.g., lead aprons, lead gloves, protective eyewear, thyroid shields, portable individualized lead panels, stationary barriers) to be used, under what circumstances, for patients, including high-risk patients as identified in radiologic services policies and procedures, patient family members or support persons who may be needed to be with the patient during a study or procedure, and hospital personnel;<br>• Lead and concrete barriers built into the walls and other structures of the imaging areas;
-
The hospital must adopt and implement written policies and procedures to ensure safety from radiation hazards. The policies and procedures must include, but are not limited to, consideration of the following:<br>• Identification and use of appropriate containers to be used for various radioactive materials, if applicable, when stored, in transport between locations within the hospital, in use, and during/after disposal.
-
Personal shielding, supplies and equipment are properly maintained and routinely inspected by the hospital.
-
Proper shielding is applied to a patient who is undergoing a procedure using ionizing radiation.
-
Staff members appropriately extricate themselves from the immediate exposure field while performing a study or procedure using ionizing radiation.
-
Staff wear shielding as appropriate, per hospital policy.
-
Any hazardous radiation materials are clearly labeled, properly stored in a safe manner in the requisite containers, and disposed of in the appropriate manner
§482.26(b)(2) - Periodic inspection of equipment must be made and hazards identified must be properly corrected.
-
The inspection records (logs) verify that periodic inspections are conducted in accordance with Federal and State laws, regulations and manufacturer’s instructions.
-
Inspection and maintenance activities were performed by qualified individuals.
-
The maintenance logs show documentation of the calibration upon installation and after major upgrades or servicing.
-
Problems identified through the testing and maintenance program are properly corrected in a timely manner and the correction is maintained over time.
§482.26(b)(3) - Radiation workers must be checked periodically, by the use of exposure meters or badge tests, for amount of radiation exposure.
-
Staff being monitored have been trained about the appropriate use and storage of their badges/meters. Staff are knowledgeable about their personal radiation exposure over various timeframes.
-
Staff in categories or locations identified for monitoring have radiation-detecting meters or badges and they appropriately wear and store them.
-
Monitoring of staff exposure is documented.
-
The hospital takes appropriate steps if staff exposure exceeds parameters established per hospital policy.
§482.26(b)(4) - Radiologic services must be provided only on the order of practitioners with clinical privileges or, consistent with State law, of other practitioners authorized by the medical staff and the governing body to order the services.
-
The medical staff and the governing body determine the necessary qualifications and clinical privileges that practitioners must have to order diagnostic radiologic studies or therapeutic procedures.
-
For outpatient services, the governing body and medical staff may also authorize practitioners who do not have hospital privileges to order such studies or procedures, as permitted under State law. For example, a hospital may decide that it will routinely accept orders from physicians in the communities it services for outpatient diagnostic studies, regardless of whether those physicians have privileges to practice in the hospital.
-
There is an order for all radiologic services, and that the order was dated/timed and authenticated by an authorized practitioner prior to the diagnostic study or therapeutic procedure being performed.
§482.54(c) Standard: Orders for Outpatient Services
-
Outpatient services must be ordered by a practitioner who meets the following conditions:<br>(1) Is responsible for the care of the patient.<br>(2) Is licensed in the State where he or she provides care to the patient.<br>(3) Is acting within his or her scope of practice under State law.<br>(4) Is authorized in accordance with State law and policies adopted by the medical staff, and approved by the governing body, to order the applicable outpatient services.<br>This applies to the following:<br>(i) All practitioners who are appointed to the hospital’s medical staff and who have been granted privileges to order the applicable outpatient services.<br>(ii) All practitioners not appointed to the medical staff, but who satisfy the above criteria for authorization by the medical staff and the hospital for ordering<br>the applicable outpatient services for their patients.
-
The hospital verifies that the order or referral comes from a referring practitioner who is appropriately licensed in the jurisdiction where he/she provides care to the patient and is practicing within his/her scope of practice under State law to prescribe such orders.
§482.26(c) – Standard: Personnel
-
(1) A qualified full-time, part-time or consulting radiologist must supervise the ionizing radiology services and must interpret only those radiologic tests that are determined by the medical staff to require a radiologist’s specialized knowledge.
-
The supervising radiologist, including, if applicable, a consultant who provides such supervision, must be privileged as a radiologist at the hospital.
-
For diagnostic radiologic services using ionizing radiation, policies and procedures must, in addition to the requirements addressed in other portions of the radiologic services CoP, identify which types of radiologic tests require interpretation by a radiologist, as opposed to another type of practitioner holding privileges; the hospital’s medical staff must approve this policy.
-
When interpretation of radiologic tests (studies) is provided via telemedicine, the radiologist interpreting the radiological test must be licensed and/or meet the other applicable standards that are required by State or local laws in the state where the hospital (and, therefore, the patient) is located.
-
The medical staff has reviewed and approved a policy identifying the types of diagnostic radiologic tests (studies) that require interpretation by a radiologist.
§482.26(c)(2) - Only personnel designated as qualified by the medical staff may use the radiologic equipment and administer procedures.
-
The medical staff must develop policies, consistent with State law, that govern the designation of all personnel who are qualified to use the radiologic equipment and perform diagnostic or therapeutic studies or procedures.
-
Only designated individuals may use the equipment and perform studies or procedures.
-
All radiologic technologists using radiologic equipment or performing studies/procedures must be designated to do so.
-
Personnel also need to know how to respond to adverse events that may occur during a radiologic study or procedure.
-
The hospital must document training completion dates and evidence of satisfactory competence. Staff that complete training but cannot demonstrate satisfactory competence must not be permitted to use radiologic equipment and/or administer procedures.
§482.26(d) Standard: Records
-
Records of radiologic services must be maintained.
-
The radiologist or other practitioner who performs radiology services must sign reports of his or her interpretations.
-
The hospital must maintain the following for at least 5 years:<br>(i) Copies of reports and printouts.<br>(ii) Films, scans, and other image records, as appropriate.
§482.53 Condition of Participation: Nuclear Medicine Services
-
Nuclear medicine services must be provided in accordance with acceptable standards of practice. Acceptable standards of practice include maintaining compliance with applicable Federal and State law and regulations governing the use of nuclear medicine, including facility licensure requirements, as well as standards and recommendations promoted by nationally recognized professional organizations.
-
If nuclear medicine services are provided under arrangement, the governing body must, in accordance with §482.12(e), ensure that the services are provided in a manner that complies with the requirements of the nuclear medicine CoP
-
The hospital must monitor the quality and safety of nuclear medicine services. Examples of nuclear medicine indicators of potential quality and safety problems could include, but are not limited to:<br>• Incidents of improper patient preparation, such as inadequate intravenous access or lack of pre-medication, such that procedures must be cancelled or reordered;<br>• Incidents of the wrong radiopharmaceutical being used, i.e., not the radiopharmaceutical prescribed for the patient, or of the wrong dose of the prescribed radiopharmaceutical being administered, or of use of the wrong route of administration for the prescribed radiopharmaceutical.<br>• Repeats of the same diagnostic studies within a short time span, which may be an indicator of poor image quality; or <br>• Diagnostic studies or therapeutic procedures performed in a manner inconsistent with the applicable hospital written protocol.
-
The hospital is also required under the QAPI CoP to track medical errors and adverse events related to nuclear medicine services. Adverse events related to nuclear medicine services must be analyzed for their causes, and preventive actions must then be undertaken.
-
The hospital’s policies, procedures, and protocols are consistent with ALARA principles.
§482.53(a) Standard: Organization and Staffing
-
(1) There must be a director who is a doctor of medicine or osteopathy qualified in nuclear medicine.
-
(2) The qualifications, training, functions and responsibilities of the nuclear medicine personnel must be specified by the service director and approved by the medical staff.
-
The hospital must describe in writing the qualifications it requires for the director of nuclear medicine services.
-
The hospital must specify in writing the qualifications, training, functions and responsibilities of each category of personnel used by the hospital, whether personnel are employees or contractors, in the delivery of nuclear medicine services. The written specifications must be developed by the Director and approved by the hospital’s medical staff. Qualifications include at a minimum, job title, education, experience, specialized training, and licensure/certification, consistent with any applicable Federal and State law.
-
There are several different categories of personnel that may typically be involved in the provision of nuclear medicine services, including (but not limited to):
• Nuclear medicine pharmacists: these individuals are pharmacists who specialize in preparing, dispensing, and distributing radiopharmaceuticals;
• Nuclear medicine technologists: these individuals are trained to administer radioactive materials and perform the specific imaging procedures and often process the images for interpretation; and
• Nuclear medicine physicists. -
The specifications must also address ongoing training for personnel.
§482.53(b) Standard: Delivery of Service
-
Radioactive materials are prepared, labeled, used, transported, stored, and disposed of in accordance with hospital policies that are based on acceptable standards of practice.
-
The hospital limits access to radioactive materials at all times.
-
The hospital maintains accurate records of the receipt, distribution, and disposal of radioactive materials, including radiopharmaceuticals.
-
If the hospital prepares radiopharmaceuticals on site, proper safety precautions are utilized to protect staff from excess radiation and once prepared, stored in appropriate containers.
-
If the radiopharmaceuticals are obtained from an outside source, the receipt and storage are appropriately tracked.
-
A clear, recognizable label for nuclear material is appropriately displayed in all relevant areas throughout the hospital and on all radioactive materials.
-
Safety precautions are followed in the operations of the nuclear medicine service and that personnel and patients maintain and wear appropriate body shielding (e.g., lead aprons, lead gloves, thyroid shields) when appropriate.
-
Staff use their dosimeters according to manufacturer’s instructions, particularly in the appropriate placement of the dosimeter on the body, as indicated on the dosimeter.
-
The hospital ensures safe transport of radioactive materials in the hospital.
-
The appropriate container protection devices—e.g., lead for gamma emitters—are being utilized for storage and administration of radioactive materials.
-
If radio pharmaceuticals are prepared in-house, determine that the preparation is performed by, or supervised by, a registered pharmacist or MD/DO.
-
Personnel records of pharmacists, MDs/DOs and nuclear medicine personnel involved in the preparation and supervision of radio pharmaceuticals have required qualifications per State law and hospital policy.
-
The hospital has policies regarding the supervision of nuclear medicine personnel and the in-house preparation of radio pharmaceuticals.
-
Radioactive materials, including radioactive waste, have appropriate storage and disposal.
-
The hospital disposes of unneeded radio nuclides and radio pharmaceuticals.
§482.53(c) Standard: Facilities
-
Equipment and supplies must be appropriate for the types of nuclear medicine services offered and must be maintained for safe and efficient performance. The equipment must be--<br>(1) Maintained in safe operating condition; and<br>(2) Inspected, tested and calibrated at least annually by qualified personnel.
§482.53(d) Standard: Records
-
The hospital must maintain signed and dated reports of nuclear medicine interpretations, consultations, and procedures.
-
The hospital must maintain copies of nuclear medicine reports for at least 5 years.
-
The practitioner approved by the medical staff to interpret diagnostic procedures must sign and date the interpretation of these tests.
-
The hospital must maintain records of the receipt and distribution of radio-pharmaceuticals. The records must specify:<br>• the type of radiopharmaceutical;<br>• the location in the hospital where it was received, stored and dispensed;<br>• the amount received or dispensed at each location;<br>• the staff member receiving or dispensing; and<br>• when applicable, how/when it is disposed of and by whom. This would also include, when applicable, the type and amount of any radiopharmaceuticals returned to the source vendor.
-
The hospital must also have policies and procedures that address how often it reviews these records and how it reconciles discrepancies between inventory on hand and records of receipt, distribution, use, disposal and/or return to the source vendor.
-
Nuclear medicine services must be ordered only by practitioners whose scope of Federal or State licensure and whose defined staff privileges allow such referrals.
EOC & Infection Control
-
Environment of Care observations:
-
Infection prevention & control observations: