Information
-
Course Name
-
Conducted on
-
Prepared by
-
Location
-
Person being observed
Instructions
BREAKING BAD NEWS
-
Breaking Bad News
-
The aim for any health-professional is to use their skills to deliver bad news clearly, honestly and sensitively in order that patients can both understand and feel supported.
One framework that healthprofessionals find helpful is that developed by Baile and Buckman (2000). The components convey the major points to be considered when giving bad news to patients and/or their relatives. These may vary according to context, the severity of the news, the people involved, time given for planning, etc.
“In general, however, the more attention that can be given to each of these points the better the eventual performance is likely to be. Above all it is necessary to plan as carefully as possible and to respect the people to whom the information is being given by listening and watching them at all stages and being responsive to their wishes and reactions, which will be diverse. It is important to realise that the environment and healthcare professionals’ behaviour will have a profound influence upon the patient and family in all respects.”
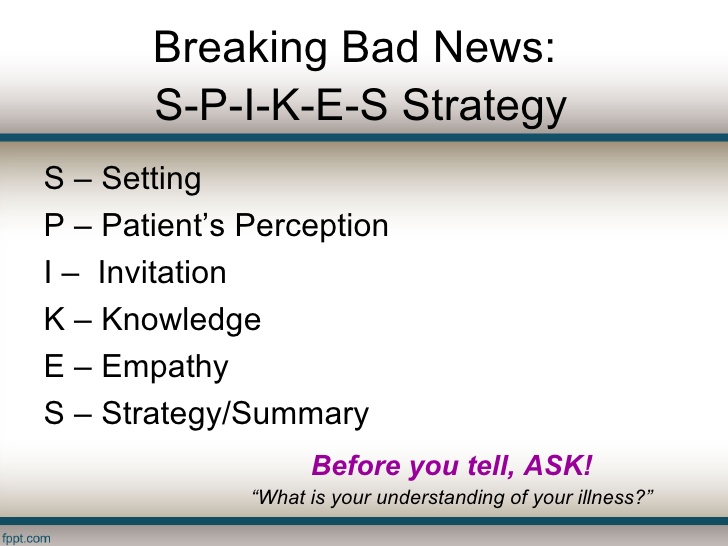
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP (2000) SPIKES – A Six-Step Protocol for Delivering Bad News: Application to the Patient with Cancer. Oncologist 5:302-311 -
SPIKES - The Six-Step Protocol for Delivering Bad News
S = SETTING up the interview
-
-
S = SETTING Up The Interview
The aim of this is to get the physical context right, maximise privacy, avoid interuption, to help patients listen and understand, respect confidentiality and provide support. Liaise with staff as necessary. The more reassured you feel about the setting the more at ease, and hence more available and helpful you will be to patient. -
All information and test results have been reviewed?
-
Decision has been made as to what terminology is to be used?
-
Team member ensures adequate privacy for the patient and their relatives?
-
Team member has discussed and/or considered the presence of other staff members and relatives, according to the patients wishes?
-
Were the introductions and opening comments appropriate? Is there anything you would change or add?
P = PERCEPTION of Condition / Seriousness
-
P = PERCEPTION of Condition/Seriousness
Finding out how much the patient knows. In particular how serious he or she thinks the illness is, and/or how much it will affect the future. -
Team member uses open ended questions to verify relatives understanding. ie. "What have you made of the illness so far? "What did doctor X tell you when he sent you here?"
-
Does the patient/relative show any signs of avoiding terminology or phrases? Are they possible signs of anxiety? (Body posture, hand movements could also be indicators)
-
What are the words that stand out to you about the patients understanding of their condition?!
-
Team member does not necessarily need to correct these behaviours, but could be useful observations in gauging how to proceed with the conversation, and to understand what is going on for the patient.
I = Obtaining the patient's INVITATION?
-
In any conversation about bad news the real issue is not "Do you want to know?" but "at what level do you want to know?"
-
Do you believe a patient has the right not to know the details of their condition?
-
It is important that the team member is able to elicit patient's wishes without imparting their own agenda. For example - "You don't want to be bothered with the details do you?" could well be considered a leading question (or an attempt for the team member to be able to avoid 'the difficult conversation').
-
How effective would you say the Team Member was at identifying the patient's wishes. Give an example of good practice or an area of improvement
-
Are you able to photograph the groups dynamics to support your observation?
-
"Would you like me to tell you the details of the diagnosis?"
K = Give KNOWLEDGE and Information to the Patient
-
How would you arrange the seating for this sort of conversation if the patient was bed bound?
-
With all the best planning, the team members need to remain pliable to the responses and needs of the patient. Does the patient's needs alter the team's pre-empted agenda for the discussion?
-
If so, please give us an example
Mirroring the patients posture and terminologies used:
-
From the terms you identified earlier, does the team positively reinforce parts which are correct about their condition?
-
How does the team member/s educate the patient and/or relatives about any misunderstandings or lack of clarity? Give examples.
-
E = Addressing the patients EMOTIONS with empathic responses
-
Responding to a patients feelings is one of the more difficult challenges in breaking bad news. Patient's responses can vary from silence to distress, denial or anger.
-
Does the Team Member -
-
allow the patient time to process the information?
-
acknowledge any shock and ask them what they are thinking/feeling?
-
use silence to allow reflection?
-
allow expression of emotion without criticism?
-
Any further observations?
S = Strategy & Summary
-
Demonstrate an understanding of the patient's problem list
-
Indicate you can distinguish the fixable from the unfixable
-
Make a Plan or Strategy and explain it
-
Preparing for the worst and hoping for the best
-
Identify coping strategies of patient and reinforce them
-
Identify other sources of support for the patient and incorporate them
-
Invite questions
-
-
In your own practice, when the patient has left:
-
Remember to check your own feelings
-
Deal with the next patient sensitively, as they may have been neglected
Conclusion
-
This brings us to the end of this peer observation and learning tool.
-
Please sign off this observation
-
Select date
-
It can be useful to email a copy of this document to yourself and those that have been observed. Go to EXPORT document and ask all necessary personel to add their email.